I believe there is an incredibly large gap in the way we approach health and wellness with a significant emphasis placed on our physical health. When something starts to go wrong physically (i.e. weight gain, blood pressure, cholesterol, pre-diabetes, depression/anxiety, etc.), we turn to physical methods to try and solve the problem. This could include changing our diet and exercise plan, starting a new medication, and the list goes on. What I hope to demonstrate in this article is that our physical health is often an outer expression of an inner conflict. Bear with me as we dive into some astounding research summarized by Jane Ellen Stevens at ACEs Too High News.
In 1985, a man named Dr. Vincent Felitti, chief of Kaiser Permanente’s revolutionary Department of Preventive Medicine in San Diego, CA, ran an obesity clinic. Anyone who wanted to shed as little as 30 pounds could participate, but the clinic was designed for people who were 100 to 600 pounds overweight. Every year, more than 50,000 people were screened for disease. It was the largest medical evaluation site in the world.
Although Dr. Felitti’s department was incredibly successful, he couldn’t figure out why, each year for the last five years, more than half of the people in his obesity clinic dropped out. After reviewing the people who had dropped out he discovered that all of these people were losing weight when they left the program. Why would someone who weighed 300 pounds, and had lost 100 of those pounds in his program, drop out? The mystery turned into a 25-year quest involving researchers from the Centers for Disease Control and Prevention and more than 17,000 members of Kaiser Permanente’s San Diego care program.
Dr. Felitti began interviewing hundreds of his clients who dropped out of this program. At first he made no progress in discovering the root of the problem until he began asking the following questions: How much did you weigh when you were born? How much did you weigh when you started first grade? How much did you weigh when you entered high school? How much did you weigh when you became sexually active? He was astonished when his first patient, a woman, replied, “Forty pounds.” And then elaborated further, “It was when I was four years old, with my father.”
A shocking 286 patients later almost all had replied in a similar manner. As startling as this was, it turned out to be less significant than another piece of the puzzle that dropped into place during an interview with a woman who had been raped when she was 23 years old. In the year after the attack, she told Felitti that she’d gained 105 pounds. “Overweight is overlooked, and that’s the way I need to be.” He realized that being overweight for these people was not a problem it was actually a solution. In the case of the woman who’d been raped, she felt as if she were invisible to men. In the case of a man who’d been beaten up when he was a skinny kid, being fat kept him safe, because when he gained a lot of weight, nobody bothered him. In the case of another woman — whose father told her while he was raping her when she was 7 years old that the only reason he wasn’t doing the same to her 9-year-old sister was because she was fat — being obese protected her. Losing weight increased these patient’s anxiety, depression, and fear to levels that were intolerable.
Over time, these results would reach far beyond an obesity clinic. They began to help explain why hundreds of millions of people around the world use biochemical coping methods – such as alcohol, marijuana, food, sex, tobacco, violence, work, methamphetamines, thrill sports – to escape intense fear, anxiety, depression, and anger. All of this led to one of the largest and perhaps most important public health studies of all time.
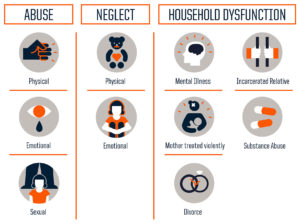
Between 1995 and 1997 a survey was filled out by 17,421 individuals coming through Kaiser Permanente’s Department of Preventive Medicine. The survey consisted of the top 10 most common adverse childhood experiences that had been reported by Dr. Felitti’s patients.
The results of this study were mind-boggling!
- There was a direct link between childhood trauma and adult onset of chronic disease, as well as mental illness, doing time in prison, and work issues, such as absenteeism.
- Two-thirds of the adults in the study had experienced one or more types of adverse childhood experiences. Of those, 87 percent had experienced 2 or more types. This showed that people who had an alcoholic father, for example, were likely to have also experienced physical abuse or verbal abuse. In other words, adverse childhood experiences(ACEs) usually didn’t happen in isolation.
- More adverse childhood experiences resulted in a higher risk of medical, mental, and social problems as an adult.
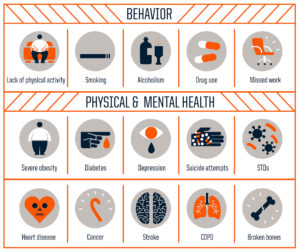
A scoring system was developed that gave each ACE one point. For example, if a person experienced verbal abuse, lived with a mentally ill mother and an alcoholic father, their ACE score was three. Compared with people with zero ACEs, those with four categories of ACEs the results were as follows:
- 240% greater risk of hepatitis
- 390% greater risk of COPD
- 240% higher risk of a sexually transmitted disease
- Twice as likely to smoke
- 12 times more likely to have attempted suicide
- 7 times more likely to be an alcoholic
- 10 times more likely to have injected street drugs
- More likely to be violent, have more marriages, more broken bones, more drug prescriptions, more depression, more auto-immune diseases, and more work absences.
To further validate the shocking results of this study, the participants were average Americans. Seventy-five percent were white, 11 percent Latino, 7.5 percent Asian and Pacific Islander, and 5 percent were black. They were middle-class, middle-aged, 36 percent had attended college and 40 percent had college degrees or higher. Since they were members of Kaiser Permanente, they all had jobs and great health care. Their average age was 57.
I think the results of this study speak for themselves, but if you are one of those people asking the question of why this really matters, let me elaborate further.
The ACE Study became even more significant with the publication of parallel research that provided the link between why something that happened to you when you were a kid could land you in the hospital at age 50. The stress of severe and chronic childhood trauma – such as being regularly hit, constantly belittled and berated, watching your father often hit your mother – put a child in constant fight or flight mode which releases hormones that physically damage a child’s developing brain. This fight or flight mode is beneficial when we’re being chased by a bear, but the real problem comes when that bear comes home from the bar every night. Constantly staying in a fight or flight mode is incredibly damaging to every aspect of our health leading to the adoption of health risk behaviors, disease, disability and early death.
The results in this study show extreme examples of what many people go through during their childhood, but that isn’t to say that other events in your life can’t have very similar effects and outcomes. Maybe you experienced trauma or loss or betrayal or abuse or disappointment at an older age. It may not physically impact your young developing brain, but the result is similar. We store these memories, try to bury them out of shame, fear, or anger and try to move on with our lives. Over time we develop ways to avoid feeling the pain. Maybe we work excessively as an avoidance tactic or form some other type of unhealthy or extreme habit to attempt to get on with life. Maybe it manifests in our relationships with our loved ones and causes a significant amount of stress on a regular basis. There are so many life events that can result in prolonged stress if we aren’t aware of or know how to deal with them in a healthy way.
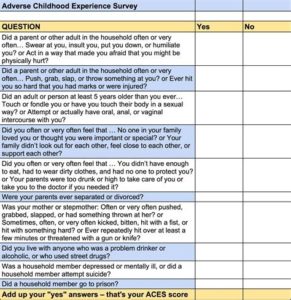
Take a second to read through the ACEs questionnaire and determine how many you may have experienced. Each time you select “yes” that counts as one ACE. This is also a good time to evaluate other experiences in your life and explore the amount of impact those experiences may still have on your everyday life and on your current and future health. It’s never too late to get help to work through past difficulties and create healthy habits so you can avoid the many pitfalls of chronic stress that lead to chronic illness, disability, and early death.
If you feel like this topic may relate to you, NOW is the time to do something about it so you don’t have to look back in the future and wonder how different your life could have been if you had taken the right steps toward better health before it was too late.
Please book a free coaching session on my contact page today to discuss available options for you to get started.
“It’s never too late to get help to work through past difficulties and create healthy habits so you can avoid the many pitfalls of chronic stress that lead to chronic illness.”